Artificial Intelligence (AI) has opened new possibilities in healthcare across Africa. In Ghana, AI-enabled tools are now being introduced in diagnostic centers, community clinics, and digital health platforms. However, there is a looming problem: most of these AI systems are not trained with data from the populations they are meant to serve.
Rural healthcare in Ghana already suffers from resource shortages, fewer specialists, and infrastructural challenges. AI is often promoted as a remedy for these inequalities. But when algorithms built on non-African datasets are used to diagnose diseases or make recommendations, they may misinterpret symptoms or produce inaccurate results. For instance, CAD4TB, an AI system for detecting tuberculosis via chest X-rays, has been deployed in some parts of Ghana. Yet, its original training data came from non-African populations. Subtle differences in anatomy, comorbidities, or even radiographic imaging quality can introduce systematic errors.
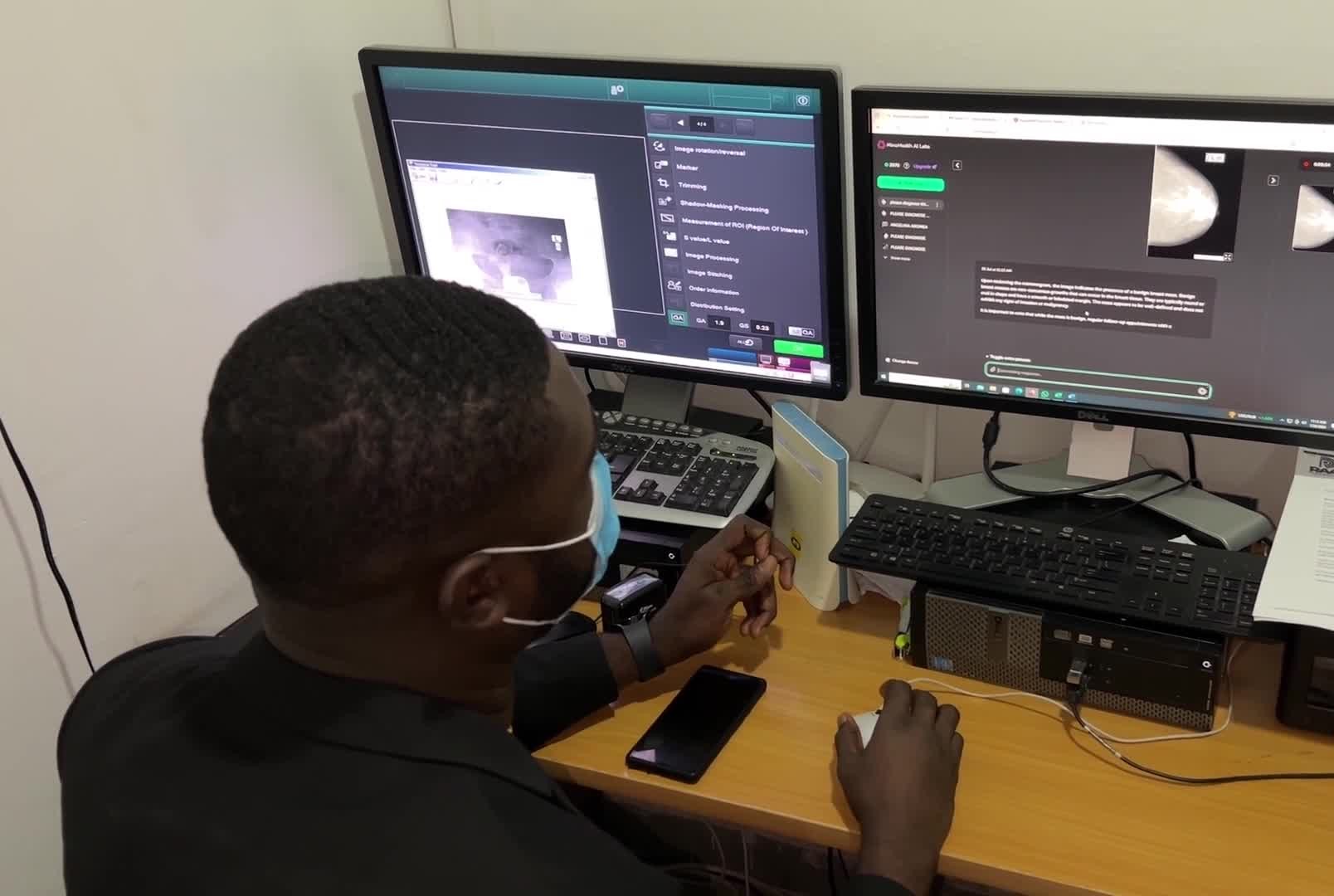
In rural settings where doctors may rely entirely on such tools, a misdiagnosis could delay treatment or lead to fatal outcomes. Moreover, without local validation studies, healthcare workers often lack the confidence to challenge AI-driven recommendations.
The risk extends beyond accuracy. Many AI systems require good-quality digital infrastructure and stable electricity—both of which are limited in many rural areas. If an AI platform fails mid-diagnosis due to a power outage or connectivity issue, there are rarely backup systems.
For AI to be effective in Ghana, especially in rural settings, developers must engage local communities, incorporate Ghana-specific health data, and pilot tools under real conditions. A one-size-fits-all approach may not only be ineffective but dangerous.